
This guest blog post was authored by Sonder Crane, MD, IBCLC, Pediatrician, Chapter Breastfeeding Coordinator-Kansas Chapter of the American Academy of Pediatrics.
“I think it’s time for mommy milk!” said my 5-year-old to my 2-year-old as their 1-month-old baby brother began to fuss. “Mommy milk” has always been the term for breast milk in our house, coined by our eldest when her sister was born.
While celebrating National Breastfeeding Month, I remember my own breastfeeding experience. I was fortunate to successfully breastfeed all three of my children. I even had enough stored milk with my oldest two children that I was able to donate to a human milk bank.


My breastfeeding journey was relatively “painless” compared to others – if you don’t count the predicted engorgement, leaking, sore nipples, thrush for both me and my infant, and associated frustrations with finding appropriate times to pump while at work. (Thankfully, I had a very understanding employer.)
As a pediatrician and International Board Certified Lactation Consultant, I also have the privilege of being part of the breastfeeding/chestfeeding journey with many of my patients and their caregivers as they work to provide nutrition for their infants. Not all of their journeys were as “painless” as mine. One case in particular stands out – a mother who came to me with her 2-month-old infant. The case was referred to me due to the infant’s poor weight gain. I worked with the mother and child over the course of about 2 years. We tried different techniques to support weight gain including different ways to give expressed breast milk, different feeding routines, elimination diets for mom, creative ways to introduce solid foods, and so many other things. We involved specialists in different fields to help support the child and mother. Ultimately, the baby did well and was growing and thriving the last time that I saw her. Her mother worked tirelessly to provide the nutrition that she needed to ensure adequate growth, even though it was not the breastfeeding journey the mother would have imagined for herself.
Why breastfeed? The importance of human milk (in brief)
Physiological Benefits to the Infant
- Human milk has been proven to be the optimal source of nutrition for infants.
- There are multiple aspects in the dynamic properties of breast milk including antimicrobial, anti-inflammatory, and immunoregulatory agents which contribute to the developing immune system of the infant and help prevent infection.
- Breastfeeding can reduce the risk of Sudden Infant Death Syndrome (SIDS), certain types of autoimmune disease (inflammatory bowel disease, diabetes mellitus, asthma, atopic dermatitis), leukemia, and obesity.
Physiological Benefits to the Mother
- The act of breastfeeding can be beneficial to maternal health in helping mothers recover more quickly from childbirth, assisting with postpartum weight loss, reducing the risk of ovarian and breast cancer, reducing the risk of hypertension, and reducing risk of type 2 diabetes.
Intangible Benefits
- Breastfeeding or chestfeeding facilitates maternal and infant bonding.
- Breastfeeding can ultimately lead to a closer and more responsive infant/mother dyad.
- It’s shown to reduce maternal stress and decrease cognitive and behavioral problems later in childhood.
What does the American Academy of Pediatrics say about breastfeeding and how do we promote and support breastfeeding mothers and their babies?
Here’s a summary of the most recently updated (July 2022) AAP Recommendations on Breastfeeding:
- Exclusive breastfeeding for the first 6 months of life (consistent with guidelines provided by World Health Organization, American College of Obstetricians and Gynecologists, American Academy of Family Physicians, and Canadian Pediatric Society)
- Continued breastfeeding along with appropriate complementary foods introduced at 6 months for as long as desired, 2+ years
- Recognize that medical contraindications to breastfeeding are rare
- Birth hospitals and centers should implement maternity care practices shown to improve breastfeeding initiation, duration, and exclusivity
- National tracking of breastfeeding rates through age 2 years
- Policies should be in place to protect breastfeeding
- Universal paid maternity leave
- Right to breastfeed in public
- Insurance coverage for necessary items and care in breastfeeding
- On-site child care in the workplace
- Universal break time and adequate accommodations for human milk expression at work
- Recognize that pediatricians (and all those caring for infants) play a critical role in breastfeeding success
- Providing evidence-based information on feeding choices
- Supporting early skin-to-skin contact and skilled lactation support while in the hospital
- Using current resources to give guidance and minimize disruptions in breastfeeding when questions arise due to maternal medications, medical conditions, or vaccinations
- Acquiring up-to-date information on the benefits of breastfeeding and how to provide breastfeeding care in the office and the community
- Advocating for culturally sensitive and appropriate policies to promote breastfeeding
- Assisting parents with preterm infants on establishing milk supply when infant is unable to feed at the breast and the use of pasteurized donor human milk
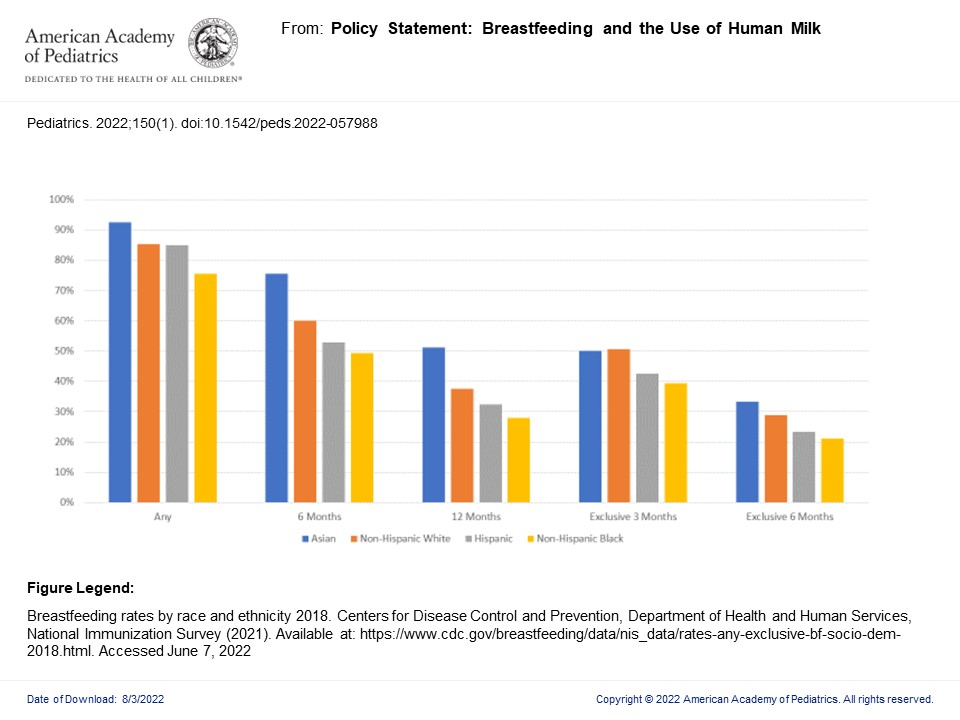
The graph above shows 2018 national breastfeeding rates for the infants in the breastfeeding dyad exclusively at 3 and 6 months of life, 6 and 12 months of life, and any breastfeeding at all throughout 0-12 months of life. Each age range is broken down into race and ethnicity at that stage. As evidenced above, we are making progress in supporting our lactating mothers and breastfeeding infants but there is always room for improvement. The education is ongoing as we strive to advocate for the breastfeeding dyad.
There are two excellent local upcoming opportunities for education as we welcome Dr. Joan Younger Meek to Grand Rounds at Wesley Medical Center in Wichita, KS, on September 15, and at the Kansas Chapter of the AAP Fall CME Meeting at Hyatt Regency Hotel in Wichita, KS, on September 16. Dr. Meek is the lead author of the new policy statement published July 2022 on “Breastfeeding and the Use of Human Milk” in the Journal of Pediatrics and a leading expert on breastfeeding and lactation. Please attend her presentations if you have the chance. In the meantime, Happy National Breastfeeding Month!
About the series
This is the third post in a series on breastfeeding in Kansas. Other posts include:
- Kansas’ breastfeeding journey: reflections and the road ahead
- The state of breastfeeding in Kansas
- How WIC supports breastfeeding
- Black women breastfeed