This guest blog post was authored by Joyea Marshall-Crowley, CBS, Wichita Black Breastfeeding Coalition.
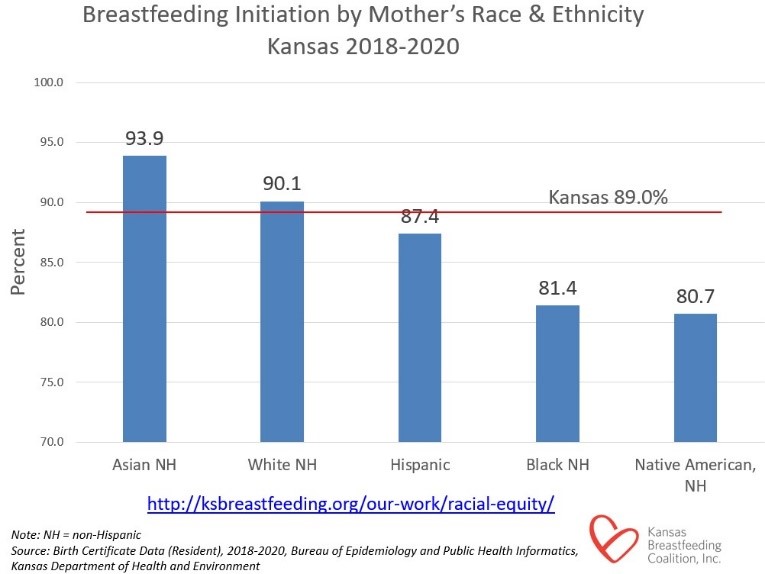
In the Wichita area, we have heard from Black and brown mothers that they are not even being asked about breastfeeding as an initial feeding choice, and that their healthcare providers assume they are formula-feeding their babies. This makes it difficult for Black and brown mothers to obtain breastfeeding resources, support, or information during pregnancy and upon delivery. It is imperative to have these supports for a woman’s breastfeeding journey, and it should be accessible to all mothers no matter their decision to breastfeed or not.
The need for the Wichita Black Breastfeeding Coalition is clear.
Who is the Wichita Black Breastfeeding Coalition?
The Wichita Black Breastfeeding Coalition (WBBC) was formed in October 2020 under the non-profit organization Kansas Breastfeeding Coalition. The foundational vision for this local breastfeeding coalition is to help increase breastfeeding rates in the Black and brown communities of the Wichita Metropolitan Area.
The coalition currently houses six members. The outstanding members of the WBBC hold many titles, such as Certified Breastfeeding Specialist (currently on track to obtain their IBCLC), Certified Trained Doulas, Registered Nurse, Chocolate Milk Certified Trainer, Chiropractor, and Midwife, to name a few.
All WBBC members share the same passion for helping women of color gain the support, resources, and tools needed to reach their breastfeeding goals. We want mothers of color to have a safe space just for them to receive the breastfeeding support they need—and that is what they will get from the Wichita Black Breastfeeding Coalition.
“I Breastfed; This is My Legacy”
Representation of Black women is so important when it comes to normalizing breastfeeding. This group is underrepresented, and there is already a stigma in the Black and brown community that breastfeeding is a “white” thing. When they see pictures and videos of breastfeeding mothers that heavily display white mothers as the focus it just reinforces the same message as the stigma and creates barriers.
To dispel this myth, the Wichita Black Breastfeeding Coalition created a project called “Latched Legacy.” This project highlights and normalizes that Black women do indeed breastfeed. The campaign video shows Black mothers confidently sharing the statement “I Breastfed; This is My Legacy” while capturing them with their children and partners. The project’s goal is not only to increase breastfeeding initiation rates in the Wichita Metro Area but also to increase media representation for Black mothers regarding breastfeeding.
In conjunction with representation, this project has also allowed us to provide breastfeeding kits for pregnant and breastfeeding mothers of color. These kits include supplies and information to encourage them to initiate breastfeeding as their first choice upon delivery. As a result, we have a success rate of 95% of mothers who have received a kit while pregnant initiating breastfeeding as their first choice of feeding after delivery.
Breastfeeding is for mothers of all backgrounds. We are changing the Black breastfeeding narrative one family at a time in the Wichita area. Every Kansas family should receive the resources and support they need to reach their breastfeeding goals. You can support new or expecting parents in your area by referring them to a local breastfeeding coalition or to an organization that provides breastfeeding resources.
About the series
This is the final post in a series on breastfeeding in Kansas. Prior posts include: