This opinion piece by Health Fund President David Jordan originally appeared in the Kansas Reflector on November 17, 2022, the second in a two-part series on current and emerging challenges and how Kansans are looking ahead to develop innovative solutions and ensure health care for generations to come.
Health care is vital for our communities — and under increasing pressure. In part 1 of this series, we looked at challenges Kansas faces in supporting the health care systems and workforce needed for our communities to thrive.
By recognizing shifting demographics, workforce challenges and changes in health care delivery, we have the opportunity to build a sustainable health care system for the future.
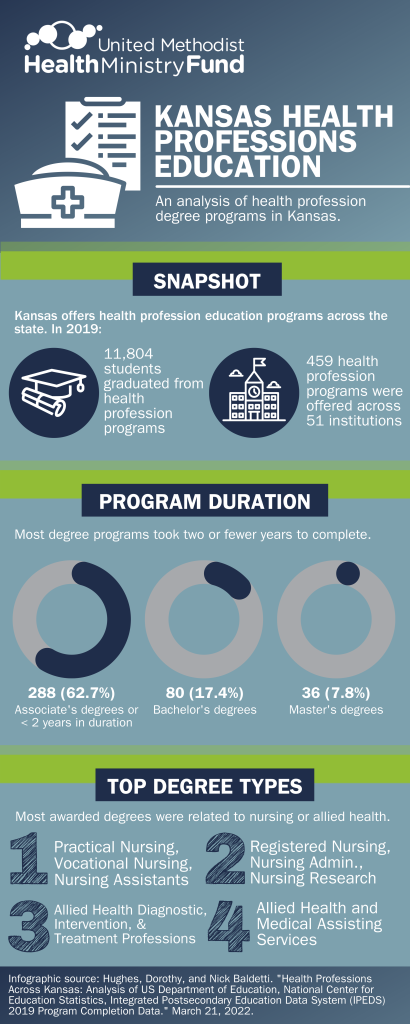
To plan ahead and better understand the health care workforce crisis, United Methodist Health Ministry Fund commissioned research examining the current health professional education pipeline in Kansas. KU School of Medicine and McPherson College researchers analyzed 2019 program completion data using the National Center for Education Statistics’ Integrated Postsecondary Education Data System (IPEDS).
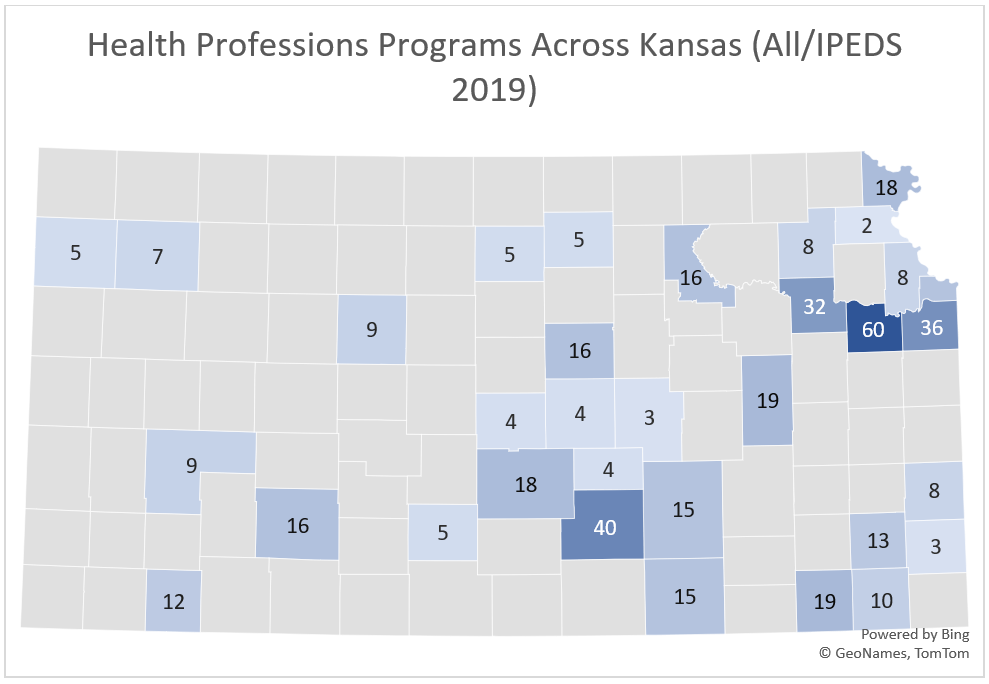
As health care faces significant staffing shortages, the report illustrates an opportunity for Kansas — with health profession programs located throughout the state — to strengthen that foundation and increase our homegrown workforce.
In 2019, 11,804 students graduated from 459 health profession programs located across 51 Kansas institutions. Most (62.7%) completed degree programs of two years or less in duration. The largest number of graduates completed degree programs in nursing or allied health.
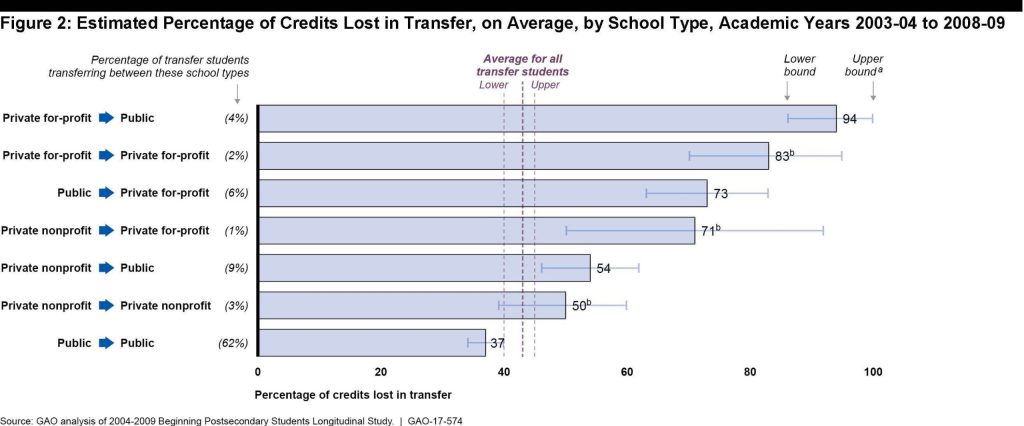
With most graduates from programs with two years or less of training, to reduce credit loss and barriers to additional training and degree attainment we need to ensure accessible transfer pathways from two-year to four-year post-secondary institutions. We also should examine policies to require credit transfers between Kansas higher education institutions.
Likewise, we need to align secondary, technical education and postsecondary education programs, and ensure health care training completed in high school is transferrable and aligned with degree programs and employer needs.
We should continue to invest in nontraditional workforce development programs such as Gov. Laura Kelly’s recently launched Office of Apprenticeship, which seeks to develop and train new talent in critical industries such as healthcare.
We need to examine scope of practice and payment policies to best use our workforce, and implement smart systems and policies enabling every provider on the team to practice to the top of their scope.
One example is the newly-recognized community health worker program in Kansas, which trains community members in a certificate program to provide crucial health coaching, resource and care coordination services, education, and navigation services. CHWs help consumers better navigate systems and reduce use of high-cost services. They allow providers to focus on practicing to the top of their scope, reducing burdens on overworked staff. While CHWs are now certified, we need to change Medicaid reimbursement policies to ensure providers can be paid for their services.
We have an opportunity to better leverage providers such as physician assistants, dental therapists and others to provide care under doctor-led teams. Expanding team members’ scope of practice can increase capacity and address workforce challenges.
We can leverage technology to maximize our workforce and better serve Kansans. Telehealth provides that opportunity. Before COVID-19, just 11% of US consumers were using telehealth, but in 2020 its unique advantages (especially in rural areas) became clear. Now, consumers and providers agree telehealth is here to stay, playing a key role in integrated, patient-centered systems of care.
Ensuring all Kansans have access to reliable broadband allows us to distribute workforce and re-design our health system in a different way. Residents can access hard-to-recruit specialty care in their communities, benefiting them while reducing burdens of recruitment. However, we must change policies to foster this innovation for the long term.
Workforce competitiveness requires a financially viable system. Kansas is one of only 11 states that has not expanded Medicaid, putting hospitals and other providers at financial risk. Expansion would eliminate high levels of uncompensated care, helping prevent further hospital closures and benefitting all Kansas health providers.
Changing needs require new approaches. Under the Rural Emergency Hospital model, hospitals continue providing emergency services and routine care but discontinue acute inpatient care.
Beyond direct workforce and health system issues, we need to ensure Kansas has community supports to ensure health care workers remain in Kansas, including child care. A 2020 study reported only 3% of Kansas counties met desired capacity — before COVID-19. While solving the child care crisis requires sustained work at all government levels, we can take steps today, including better use of child care subsidies.
There is no single solution. Increasing our health care workforce requires research, collaboration, policy change and willingness to change the status quo. Kansans, working together, can ensure our communities have health care and thrive for generations. Join the conversation at https://communityconversationsks.com.
Back to All News